
DRY EYE
LEARN MORE ABOUT DRY EYE
Are you frustrated with how your eyes feel? Do you want answers and results? You're in the right place.

Do You Have Dry Eye?
Dry eye presents differently in every patient; therefore we take an individualized approach to your care. You may have dry eye if you experience:
Dryness, Grittiness, Scratchiness, Irritation, or Foreign Body Sensation
Excessive Tearing, Crusting or Debris, Redness, Styes, Irritated eyelids
Worsening or Fluctuating Vision, Frequent Prescription Changes, Intolerance to Contacts
Glare, Sensitivity to Light, Eye Fatigue, Headaches, or Double Vision (That Does Not Improve When Covering One Eye)
What To Expect At Your Dry Eye Evaluation
Your one hour long dry eye evaluation will start with a comprehensive history. You will be asked to fill out a questionnaire about your symptoms, lifestyle, medical history and medications, diet, and previous therapies. We use this information to coach you on changes you can make during your daily life to improve your symptoms. We discuss what has worked for you, and what has not, to avoid recreating the wheel.
We will then perform a series of tests to identify other underlying causes such as ocular inflammation, poor tear production, incomplete lid closure, allergies, mites or bacteria, clogged oil glands, low omega levels, tear evaporation, and more.
We wrap up the appointment by reviewing your results and connecting the dots between your causes and symptoms. We outline a treatment plan and discuss how each treatment works, how long it takes to be effective, and any potential side effects. You will be given samples, products, and a treatment guide with instructions leaving you feeling empowered to tackle your dry eye.

.avif)
What Is Dry Eye?
"Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles" as defined by the DEWS 2.
There are three layers to the tear film: Mucin, Aqueous, and Lipid. The bottom mucin layer is secreted by cells in the conjunctiva, and acts to keep tears on the eye. The middle aqueous layer is secreted by the lacrimal gland, and is the bulk of the tear film. The top lipid layer is secreted by meibomian glands in the eyelid to prevent the tears from evaporating.
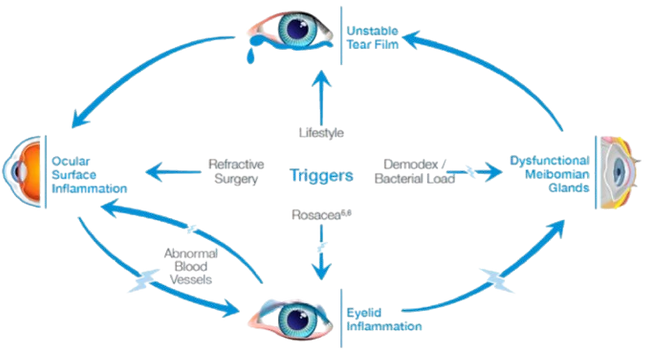
There are many reasons that the tear film can become dysfunctional, causing dryness of the ocular surface. Damaged tissue releases inflammation which causes more tissue damage, and the cycle worsens. For this reason, we classify dry eye as a chronic inflammatory condition.
Common Causes of Dry Eye
Find The Root Cause
Dry Eye is a multifactorial condition, which is why we perform an extensive evaluation to determine what is causing your symptoms. This allows us to treat the problem at the source. The list below is not exhaustive.

Resources
Treating dry eye can be challenging, but we are here to support you.
-
Intense Pulsed LightThe Lumenis OptiLight IPL (Intense Pulsed Light) is a non-invasive treatment designed to help manage and treat dry eye disease (DED), particularly when the underlying cause is meibomian gland dysfunction (MGD). MGD is a common condition where the meibomian glands in the eyelids do not produce enough oil (lipid) for the tear film, leading to evaporative dry eyes. The OptiLight IPL treatment uses pulses of light to improve the function of these glands and address dry eye symptoms. Key Features of Lumenis OptiLight IPL: Intense Pulsed Light (IPL) Technology: The OptiLight system uses intense pulsed light, which delivers light energy in multiple wavelengths to the skin around the eyes. The light energy is absorbed by the meibomian glands and helps to liquefy and clear blockages in these glands, improving their function and increasing the flow of the oil necessary for a healthy tear film. Targeting Meibomian Gland Dysfunction (MGD): The treatment is specifically effective in cases of MGD, a leading cause of dry eye disease, as it helps restore the function of the meibomian glands and reduce gland obstruction. By improving the oil component of the tear film, it helps to stabilize the tear film, reduce evaporation, and alleviate symptoms like dryness, irritation, and burning. Comfort and Safety: The procedure is generally safe and well-tolerated, with mild discomfort during the treatment. A cooling gel is often applied to the skin to enhance comfort during the procedure. The IPL treatment is also designed to minimize side effects, with few reports of complications when used by trained professionals. Non-Surgical and Non-Invasive: OptiLight IPL is a non-surgical, non-invasive procedure that does not require any incisions or injections. It involves applying light pulses to the skin on the lower eyelids, targeting the meibomian glands indirectly. How Lumenis OptiLight IPL Works: Light Energy Application: During the treatment, a specialized handpiece is used to deliver pulses of light to the skin around the eyes, specifically the area of the eyelids where the meibomian glands are located. Improves Meibomian Gland Function: The light energy targets the meibomian glands and helps to break down the blockages in the glands, which can be caused by thickened oil. The heat and light work to soften the oil and help the glands expel it. Improves Tear Film Quality: As the meibomian glands become more functional, they begin to produce a healthier oil layer in the tear film. This helps to stabilize the tear film, reduce evaporative dry eye, and relieve symptoms associated with dry eye disease. Stimulates Skin Rejuvenation: IPL may also help stimulate collagen production and improve the health of the skin around the eyes. This contributes to overall skin rejuvenation and may improve the appearance of fine lines and wrinkles around the eye area. Treatment Process: Pre-Treatment: Before the procedure, the eye area is typically cleaned and a cooling gel may be applied to protect the skin and enhance the light's effectiveness. IPL Application: The IPL handpiece is placed near the skin around the eyes, and pulses of light are delivered to the treatment area. The light is absorbed by the targeted tissues, including the meibomian glands. Duration: The procedure typically lasts around 15-20 minutes and can be done in a clinical setting by a trained professional, such as an ophthalmologist or optometrist. Post-Treatment Care: After the treatment, there is generally no downtime. Patients may experience mild redness or warmth in the treated area, but these side effects typically resolve quickly. Some patients may be advised to continue with other forms of treatment for dry eye disease, such as lubricating eye drops or eyelid hygiene routines, to support the results. Benefits of Lumenis OptiLight IPL: Improves Meibomian Gland Function: The primary benefit of OptiLight IPL is its ability to improve meibomian gland function, helping to restore proper oil production in the tear film and reducing symptoms of dry eye disease caused by MGD. Non-Invasive: Unlike surgeries or injections, IPL is a non-invasive, painless treatment that can be performed in a short amount of time with minimal discomfort. Improves Dry Eye Symptoms: Many patients report significant improvement in dry eye symptoms, including reduced dryness, irritation, burning, and discomfort, following a series of IPL treatments. Long-Term Relief: Although results vary, many patients experience long-lasting relief from dry eye symptoms, with improvement often lasting for several months. Skin Benefits: In addition to improving meibomian gland function, IPL can also have aesthetic benefits, such as reducing fine lines and improving skin texture around the eyes due to its collagen-stimulating properties. Potential Side Effects: While Lumenis OptiLight IPL is generally considered safe, there are some potential side effects to be aware of: Mild Redness or Warmth: The skin around the eyes may feel warm or appear slightly red immediately after treatment, but this usually resolves quickly. Temporary Swelling: Some patients may experience mild swelling around the eyes following treatment. Light Sensitivity: IPL treatment can make the skin more sensitive to light, so patients are often advised to avoid direct sun exposure after the procedure. Eye Sensitivity: Although rare, some patients may experience temporary discomfort in the eyes. Treatment Schedule: The number of treatments needed varies by individual. Typically, a series of 3-4 sessions is recommended, spaced 3-4 weeks apart for optimal results. Maintenance treatments may be suggested every 6-12 months, depending on the patient's needs and the severity of their dry eye disease. Conclusion: Lumenis OptiLight IPL is an innovative, non-invasive treatment for managing dry eye disease, especially when caused by meibomian gland dysfunction. By using intense pulsed light, it helps improve meibomian gland function, reduce inflammation, and restore proper oil production in the tear film, providing lasting relief from dry eye symptoms. With minimal downtime and relatively few side effects, it offers a promising option for patients who have not found relief with traditional treatments for dry eyes. Always consult with an eye care professional to determine if OptiLight IPL is right for your dry eye treatment plan.
-
Punctal PlugsPunctal plugs are a treatment option for people with aqueous deficient dry eye, a condition in which the eyes do not produce enough tears to keep the ocular surface properly lubricated. These plugs are small devices inserted into the puncta — the small openings on the eyelids that drain tears into the nasal cavity. By blocking or reducing the drainage of tears, punctal plugs help to retain more of the natural tears that are produced, offering relief from the dryness, irritation, and discomfort that come with dry eye disease. There are two main types of punctal plugs used to treat aqueous deficient dry eye: silicone plugs and collagen plugs. Both types work to improve tear retention, but they have different materials, characteristics, and durations of effectiveness. 1. Silicone Punctal Plugs Silicone plugs are a popular and commonly used type of punctal plug, particularly for those with chronic dry eye or aqueous deficient dry eye. These plugs are made of a flexible, durable silicone material that is designed to stay in place for a long time. Key Features of Silicone Punctal Plugs: Long-Term Solution: Silicone plugs are permanent (or semi-permanent) and typically do not need to be replaced often. Once inserted, they can stay in the punctum for months or even years, depending on the patient’s condition and the type of plug used. Retention of Tears: Silicone punctal plugs are designed to block tear drainage more effectively, which helps to increase the amount of tear film available on the surface of the eye, providing long-lasting moisture and reducing symptoms of dry eye. Customizable Fit: Silicone plugs come in various sizes and shapes, allowing for customization to fit the individual patient's anatomy and needs. Some plugs are designed to be adjustable, allowing for fine-tuning after insertion. Permanent or Refillable: These plugs are generally designed to be permanent, though some are removable or may need to be adjusted over time. They are inserted by an eye care professional and can be removed if necessary. Advantages: Long-lasting relief from dry eye symptoms. Minimal maintenance required. Reduces the need for frequent artificial tear use. Can be used in both lower and upper puncta (tear drainage openings). Disadvantages: Not suitable for all patients, especially those with punctal scarring or other anatomical issues. In rare cases, the plug may cause irritation, infection, or become displaced. Overplugging (blocking both puncta) can cause excessive tearing or discomfort in some patients. Procedure: Silicone punctal plugs are usually inserted in an in-office procedure by an ophthalmologist or optometrist. The procedure involves inserting the plugs into the puncta using specialized instruments. Local anesthetic drops may be used to numb the area, ensuring the procedure is painless. 2. Collagen Punctal Plugs Collagen punctal plugs are another type of punctal plug, made from a biodegradable collagen material. These plugs are typically used as a temporary solution for dry eye management, often for those who are new to punctal plugs or for those who want to test the effectiveness of the treatment before committing to permanent silicone plugs. Key Features of Collagen Punctal Plugs: Temporary Solution: Collagen plugs dissolve over time, usually within a few days to weeks. This makes them ideal for patients who want to test the efficacy of punctal plugs before opting for a more permanent solution like silicone plugs. Less Durable: Since collagen plugs are designed to dissolve, they do not provide the long-term relief that silicone plugs offer. However, they can still help reduce dry eye symptoms for the duration they remain in place. Biodegradable: The collagen material gradually breaks down and is absorbed by the body, meaning patients do not need to worry about the plugs needing removal. This makes them a low-maintenance option. Reduced Risk of Overplugging: Because they are temporary, collagen plugs reduce the risk of complications like excessive tearing or discomfort from overplugging. Advantages: Temporary, offering a trial period to assess whether punctal plugs are effective. Biodegradable, so no removal is necessary. Minimal risk of side effects since they are designed to dissolve naturally. Can be an ideal choice for patients who are uncertain about long-term treatment. Disadvantages: Short-term effectiveness, requiring replacement if long-term relief is desired. May not be suitable for patients with severe dry eye who require long-lasting moisture retention. Requires more frequent replacements compared to silicone plugs. Procedure: Like silicone plugs, collagen plugs are inserted by an eye care professional in an office setting. The process is similar, with the plugs being inserted into the puncta using specialized tools. Local anesthesia is typically used to ensure comfort during the procedure. Choosing Between Silicone and Collagen Punctal Plugs: The choice between silicone and collagen punctal plugs depends on the patient's specific condition, treatment goals, and preference: Silicone Punctal Plugs: Best for individuals with chronic dry eye or those who need long-term relief. Ideal for patients who do not want frequent replacements. Suitable for both lower and upper puncta. Collagen Punctal Plugs: Ideal for temporary relief or for patients who want to test the efficacy of punctal plugs. Best for those who prefer a non-permanent solution or who have relatively mild dry eye. More suitable for individuals who may want to evaluate the effect of punctal plugs without committing to a permanent solution. Benefits of Punctal Plugs for Aqueous Deficient Dry Eye: Increased Tear Retention: By blocking the puncta, these plugs reduce tear drainage, which helps retain more of the body’s own tears and increases moisture on the ocular surface. Improved Comfort: Many patients with aqueous deficient dry eye report improved comfort and reduced symptoms of dryness, burning, and irritation after using punctal plugs. Reduction in Artificial Tear Use: Punctal plugs can decrease the need for frequent use of artificial tears or other lubricating eye drops, leading to greater convenience. Non-Invasive: The procedure is minimally invasive and is performed in-office without the need for surgery or lengthy recovery times. Potential Risks and Side Effects: Discomfort: Some patients may experience discomfort or a feeling of pressure after the insertion of punctal plugs, especially if the plugs do not fit properly. Infection: Though rare, there is a slight risk of infection or inflammation at the site of insertion. Displacement: The plugs may become displaced or fall out, especially if they are not securely fitted. This is more common with temporary collagen plugs. Excessive Tearing: In rare cases, punctal plugs can cause excessive tearing (epiphora) if too many tears are trapped in the eye, leading to discomfort. Allergic Reactions: Some individuals may have allergic reactions to the material of the plugs, although this is uncommon. Conclusion: Punctal plugs, whether silicone or collagen, are effective treatments for aqueous deficient dry eye, especially when meibomian gland dysfunction is the underlying cause. Silicone plugs provide long-term relief, while collagen plugs offer a temporary solution for testing effectiveness. Both options are minimally invasive and have proven to improve comfort and reduce symptoms associated with dry eye disease. Working with an eye care professional is essential in determining the best type of punctal plug and ensuring proper insertion and monitoring for optimal results.
-
Lid Cleaning TreatmentsZest by Zocular is a lid hygiene and ocular health product designed to help manage and maintain the health of the eyelids and lashes, particularly for those suffering from dry eye disease, blepharitis, and meibomian gland dysfunction (MGD). It contains okra-based ingredients and is marketed as a gentle, natural solution for eyelid hygiene and maintaining the health of the eyelid and ocular surface. Key Features of Zest by Zocular: Okra-Based Formula: Zest is formulated with okra extract, which is a natural ingredient known for its soothing, hydrating, and anti-inflammatory properties. Okra is rich in mucilage, a gel-like substance that helps moisturize and calm the eyelid area, and it is used for its potential ability to remove debris, reduce inflammation, and improve lubrication around the eyes. Cleansing and Hygiene: Zest provides a gentle, yet effective, eyelid cleanse, helping to remove dirt, oil, and debris from the eyelids and lashes. This is particularly important for individuals with conditions like blepharitis, where the eyelid margins may become inflamed due to bacteria, oils, or debris. Supports Healthy Meibomian Glands: By improving eyelid hygiene, Zest can help with meibomian gland dysfunction (MGD), a leading cause of evaporative dry eye. MGD occurs when the oil-producing glands in the eyelids become blocked, causing tears to evaporate too quickly and leading to dry eye symptoms. Keeping the eyelids clean and clear of debris supports proper meibomian gland function. Soothing and Non-Irritating: The okra extract in Zest is soothing and non-irritating, making it suitable for individuals with sensitive skin or eyes. It can provide relief from discomfort, itching, and inflammation around the eyes, which are common symptoms of dry eye disease or blepharitis. Convenient and Easy to Use: Zest is available in a foam or wipe format, making it easy to use as part of a daily eyelid hygiene routine. It can be applied directly to the eyelids and lashes, offering a simple way to maintain eyelid cleanliness and ocular health. Benefits of Zest by Zocular: Cleanses and Refreshes: Zest helps to gently clean the eyelid area without harsh chemicals, alcohol, or preservatives. This gentle cleaning action helps reduce inflammation and irritation, keeping the eyelid and lash line clear of debris and oils that can contribute to dry eye symptoms. Supports Tear Film Health: By promoting a healthy eyelid environment, Zest can help improve the stability of the tear film, which is essential for maintaining moisture on the ocular surface. This is particularly beneficial for individuals with aqueous deficient dry eye or meibomian gland dysfunction (MGD), as a clean lid environment can aid in the proper functioning of the tear glands. Reduces Symptoms of Blepharitis: Zest is particularly useful for people with blepharitis, a condition where the eyelids become inflamed, often due to bacterial growth or blocked glands. By regularly cleaning the eyelids and removing bacteria or excess oils, Zest can help reduce symptoms like redness, swelling, itching, and discomfort. Natural and Gentle: With its natural okra-based ingredients, Zest is a gentler alternative to harsher cleaning products that may contain alcohol or preservatives, making it suitable for individuals with sensitive eyes or skin around the eyelids. How to Use Zest by Zocular: Foam: Shake the bottle gently before use. Apply a small amount of the foam to a clean cotton pad, gauze, or directly to the eyelids. Gently massage the foam onto the eyelid area and the lash line, ensuring to remove any debris, oil, or dirt. Rinse the area with lukewarm water or wipe with a clean tissue, if necessary. Wipes: If using the pre-moistened wipes, simply use one wipe to gently clean the eyelids and lashes. Wipe along the eyelid margins and lash line to remove any buildup of oils or debris. Discard the wipe after use. Potential Side Effects and Considerations: Minimal Irritation: Zest is generally well-tolerated and designed for sensitive skin around the eyes. However, if irritation or redness occurs, discontinue use and consult an eye care professional. Contact Lenses: If you wear contact lenses, it’s advisable to remove them before using Zest, as the product may contain ingredients that could interact with your lenses. Consistency: For optimal results, use Zest regularly as part of your daily eyelid hygiene routine. The product is usually recommended for daily use, and consistency is key to managing dry eye symptoms and maintaining healthy eyelids. Conclusion: Zest by Zocular is a gentle, okra-based eyelid treatment designed to support ocular health and dry eye management by improving eyelid hygiene and promoting the health of the tear film. It is particularly useful for individuals with meibomian gland dysfunction (MGD), blepharitis, and aqueous deficient dry eye, offering a natural, soothing alternative to harsher chemical-based eyelid treatments. By cleansing the eyelid area, reducing inflammation, and improving gland function, Zest can help alleviate symptoms of dry eyes and contribute to overall eye comfort.
-
Gland ExpressionGland expression is a common and effective treatment for Meibomian Gland Dysfunction (MGD), a condition where the Meibomian glands in the eyelids fail to produce an adequate amount of oil (meibum) needed to form a stable tear film. This dysfunction leads to dry eye symptoms, irritation, and discomfort, as the tear film becomes unstable and evaporates too quickly. What is Meibomian Gland Dysfunction (MGD)? MGD occurs when the Meibomian glands, located in the upper and lower eyelids, become blocked or inflamed, preventing them from secreting the oil that helps lubricate and protect the surface of the eye. Without this oily layer, the tears evaporate too quickly, leading to dryness, itching, burning, redness, and even blurry vision. The blockage can be caused by various factors, such as: Inflammation of the glands Thickened meibum (the oil produced by the glands) Reduced blinking frequency Hormonal changes Aging Environmental factors (dry air, wind) What is Gland Expression? Gland expression refers to the process of releasing the built-up oils (meibum) from the Meibomian glands to restore proper functioning. The procedure is performed by an eye care professional (optometrist or ophthalmologist) and aims to clear the blockages in the glands and improve oil production. There are two main types of gland expression: Manual Gland Expression: This method involves the gentle manual expression of the Meibomian glands using pressure on the eyelids. The eye care provider will typically use their fingers or a specialized tool to apply gentle pressure along the eyelids (near the lash line). This helps push the thickened oils out of the glands. Manual expression is often done after warming the eyelids (using a warm compress or specialized device) to soften the meibum, making it easier to express the oils. Thermal Pulsation Devices (e.g., LipiFlow): Thermal pulsation systems, such as LipiFlow, are often used to treat MGD by combining heat and gentle pressure to open the Meibomian glands and help release the thickened oil. These devices are FDA-approved and use controlled heat and pulsatile pressure to treat the glands without direct manual pressure. The heat softens the meibum, while the pulsatile pressure helps express the oils from the glands. LipiFlow, for example, involves placing a device on the eyelids, which applies precise heat to the inner eyelids while also delivering gentle pressure to the glands. Benefits of Gland Expression for MGD: Improved Tear Film Stability: By expressing the oils from the Meibomian glands, gland expression helps restore the lipid layer of the tear film, which reduces tear evaporation and improves eye lubrication. This results in relief from dry eye symptoms like burning, itching, and redness. Relieves Symptoms of Dry Eye: Gland expression can provide immediate relief from the discomfort associated with MGD by improving the oil flow to the surface of the eye and reducing inflammation in the eyelids. Enhances Oil Production: Regular gland expression can help stimulate the Meibomian glands and encourage healthier oil production. This can lead to long-term relief from dry eye symptoms and improve overall eye health. Reduces Eye Inflammation: Gland expression may help reduce inflammation around the glands and the eyelid area, which can further reduce symptoms like redness and swelling of the eyelids. Quick and Non-Invasive: Both manual gland expression and thermal pulsation treatments are non-invasive and relatively quick, with most treatments taking around 15-30 minutes. There is minimal discomfort involved, and the procedure is typically well-tolerated. How Gland Expression Is Performed: Preparation: The process usually begins with a warm compress or the use of a specialized heat system (such as a heat mask) applied to the eyes to soften the meibum. This helps make the oil easier to express. Expression: In the case of manual expression, the provider will apply gentle pressure to your eyelid, either with their fingers or using a specialized tool designed for this purpose. For thermal pulsation systems like LipiFlow, the device will be placed on the eyelids to deliver heat and pulsatile pressure, helping to express the oils from the glands. Post-Procedure Care: After the procedure, your provider may recommend lubricating drops to keep your eyes hydrated and soothe any mild discomfort. Some individuals may experience mild tenderness or a feeling of fullness in the eyelids after the procedure, but these symptoms are typically short-lived. Frequency of Gland Expression: The frequency of gland expression can vary depending on the severity of MGD and the individual’s response to treatment. Typically, several sessions may be required over a period of weeks to achieve long-lasting results. Some patients may need maintenance treatments every few months, while others may only need periodic expression. Your eye care professional will be able to recommend the best treatment plan based on the severity of your MGD and any underlying conditions. Other Treatments to Complement Gland Expression: Gland expression is often used in combination with other treatments to manage MGD effectively: Warm compresses: Regular use of a warm compress helps soften the meibum and prevent future blockages. Lid hygiene: Cleaning the eyelids regularly with lid scrubs or hypochlorous acid-based wipes can help remove debris and bacteria that contribute to MGD. Omega-3 fatty acids: Supplements rich in omega-3s (such as fish oil) can help improve the quality of the oils produced by the Meibomian glands. Anti-inflammatory medications: Medications such as cyclosporine A (Restasis) or lifitegrast (Xiidra) can reduce inflammation in the eyes. Punctal plugs: If dry eye is severe, punctal plugs can be used to block the tear drainage ducts, helping retain moisture on the eye's surface. Potential Side Effects of Gland Expression: While gland expression is generally safe, some people may experience mild discomfort, redness, or irritation of the eyelids immediately after the procedure. These symptoms are typically temporary and should resolve quickly. In rare cases, there may be pain or swelling of the eyelids, but this is uncommon. If any unusual symptoms occur, it is important to consult your eye care provider. Conclusion: Gland expression is a highly effective treatment for Meibomian Gland Dysfunction (MGD), helping to improve the flow of oils from the Meibomian glands, restore tear film stability, and alleviate the symptoms of dry eye. By combining gland expression with other management strategies like warm compresses, lid hygiene, and anti-inflammatory treatments, many individuals can find significant relief from their MGD symptoms and improve their eye comfort and health. Always consult with your eye care provider to determine the best treatment plan for your specific needs.
-
Scleral Contact LensesScleral lenses are a highly effective treatment option for individuals with dry eye disease, particularly for those with severe or chronic dry eyes that are not easily managed with artificial tears or other conventional treatments. These lenses are large-diameter, gas permeable contact lenses that vault over the entire cornea and rest on the sclera (the white part of the eye), providing unique benefits for dry eye sufferers. Here’s a breakdown of how scleral lenses work and why they are often used for treating dry eye disease: How Scleral Lenses Help with Dry Eye: Tear Reservoir: One of the primary benefits of scleral lenses for dry eye treatment is that they create a tear reservoir between the lens and the cornea. The space between the lens and the cornea fills with saline solution or a lubricating solution, which provides constant hydration and protection to the corneal surface. This helps to alleviate dryness and discomfort because the tear film is maintained throughout the day, reducing symptoms like dryness, burning, and irritation. Protection of the Cornea: Scleral lenses provide a protective barrier over the cornea, shielding it from the environment, allergens, and irritants that can exacerbate dry eye symptoms. For patients with ocular surface disease or damaged corneas, scleral lenses offer much-needed protection. Stable Tear Film: Dry eye is often caused by an unstable tear film, which leads to evaporation of tears and inadequate lubrication of the ocular surface. Scleral lenses help stabilize the tear film by reducing evaporation and maintaining moisture under the lens, ensuring more consistent hydration. Relief for Aqueous Deficient Dry Eye: Scleral lenses are particularly beneficial for people with aqueous deficient dry eye, where the eyes do not produce enough tears. The lens acts as a reservoir of fluid, supplying moisture to the eye even in the absence of sufficient natural tear production. Meibomian Gland Dysfunction (MGD) Relief: Meibomian gland dysfunction (MGD) is a leading cause of dry eye, where the oil-producing glands in the eyelids become blocked, leading to rapid evaporation of tears. Scleral lenses can help minimize tear evaporation and provide relief from the dryness caused by MGD by creating a sealed moisture environment on the eye surface. Comfort for Severe Dry Eye: Traditional contact lenses often worsen dry eye symptoms because they draw moisture away from the eye, leading to increased discomfort. In contrast, scleral lenses provide a consistent moisture supply, which can be extremely beneficial for individuals with severe or chronic dry eye conditions. Types of Dry Eye Conditions Treated with Scleral Lenses: Aqueous Deficient Dry Eye: This type of dry eye is caused by an insufficient quantity of tears produced by the lacrimal glands. Scleral lenses help by creating a tear reservoir that hydrates the cornea, reducing symptoms of dryness and discomfort. Meibomian Gland Dysfunction (MGD): MGD occurs when the oil-producing glands in the eyelids become blocked or produce insufficient oil, leading to rapid evaporation of the tear film. Scleral lenses can help by stabilizing the tear film and preventing evaporation, offering relief from this condition. Blepharitis: This is inflammation of the eyelid margins, which can contribute to dry eye symptoms. Scleral lenses can protect the ocular surface and provide moisture, offering comfort to individuals with blepharitis. Post-Surgical Dry Eye: After certain eye surgeries, such as LASIK or cataract surgery, patients may experience dry eye. Scleral lenses can provide relief by creating a stable tear reservoir and protecting the healing cornea. Keratoconus: Scleral lenses are particularly effective for individuals with keratoconus, a condition where the cornea becomes thin and irregularly shaped. The lens creates a smooth optical surface and helps stabilize tear distribution, providing comfort and visual clarity. Autoimmune Diseases: Conditions like Sjogren’s syndrome can cause severe dry eye symptoms. Scleral lenses are often recommended for these patients to provide long-lasting hydration and comfort. How Scleral Lenses Are Fitted: Custom Fit: Unlike standard contact lenses, scleral lenses are custom-designed for each patient’s eye. A detailed fitting process is necessary to ensure that the lens is the correct size and curvature to provide optimal comfort and vision. The fitting process includes measuring the corneal shape and scleral curvature using specialized equipment. Tear Film Evaluation: The eye care professional will also evaluate the tear film to ensure that the lens creates an adequate tear reservoir to keep the cornea hydrated. The lens should create a fluid layer between the lens and the eye, which is essential for alleviating dry eye symptoms. Trial Lenses: During the fitting process, trial lenses are used to assess comfort and the amount of tear film under the lens. Adjustments are made to ensure the lens provides the best fit and most effective moisture retention. Benefits of Scleral Lenses for Dry Eye: Long-Lasting Comfort: Scleral lenses provide prolonged comfort throughout the day because they create a stable tear reservoir under the lens. For patients with severe dry eye, this consistent moisture is invaluable for relieving irritation and discomfort. Improved Vision: In addition to providing comfort, scleral lenses can improve vision, particularly for individuals with irregular corneas (e.g., keratoconus) or scarring caused by dry eye disease. The lens creates a smooth surface, improving optical clarity. Protection from Environmental Irritants: Scleral lenses shield the cornea from irritants like dust, smoke, or allergens, which can exacerbate dry eye symptoms. The lens also acts as a physical barrier to the environment, providing added protection for the eyes. Reduction in the Need for Artificial Tears: Many patients who use scleral lenses experience a reduced need for frequent use of artificial tears, as the lenses provide constant moisture to the eye. This can be particularly beneficial for patients who struggle with the high frequency of artificial tear instillation. Improved Quality of Life: For patients with severe dry eye, scleral lenses can dramatically improve quality of life by reducing discomfort and restoring normal vision. They are especially helpful for individuals who have not found sufficient relief with other treatments. Potential Challenges: Initial Fitting Process: The fitting of scleral lenses can be more complex than regular contact lenses, requiring specialized expertise. Patients must work closely with an eye care professional to ensure an optimal fit. Care and Maintenance: Scleral lenses require proper cleaning, disinfection, and regular maintenance to ensure they remain safe and effective. Some patients may find this routine more demanding compared to traditional contact lenses. Cost: Scleral lenses can be more expensive than standard contact lenses, especially because they are custom-made and may require additional fittings and follow-up appointments. However, many patients find that the benefits in terms of comfort and symptom relief make the cost worthwhile. Conclusion: Scleral lenses are an excellent option for treating dry eye disease, especially for individuals with severe or chronic dry eyes that are caused by conditions like aqueous deficient dry eye, meibomian gland dysfunction, or autoimmune diseases. These lenses create a protective, moisture-retentive reservoir that keeps the cornea hydrated throughout the day, providing relief from dryness, irritation, and discomfort. Though they require a detailed fitting process and proper care, the benefits of scleral lenses for dry eye sufferers—such as long-lasting comfort, improved vision, and reduced dependency on artificial tears—make them a highly effective solution for managing dry eye symptoms.
-
RadiofrequencyRadiofrequency (RF) therapy is a relatively new and innovative treatment option for managing dry eye disease (DED), especially when it's associated with Meibomian Gland Dysfunction (MGD), one of the most common causes of dry eye. RF therapy uses targeted heat energy to treat the glands and improve tear film stability, providing relief from symptoms such as dryness, irritation, and discomfort. What is Radiofrequency Therapy for Dry Eye? Radiofrequency therapy for dry eye involves the application of radiofrequency energy (a form of electrical energy) to the eyelids and surrounding tissues. This energy generates heat that is used to warm the Meibomian glands and the eyelid tissues, aiming to melt thickened meibum (the oil produced by the glands) and stimulate better gland function. The primary goal is to improve the production and flow of the oils from the Meibomian glands to stabilize the tear film and reduce dry eye symptoms. How Does Radiofrequency Therapy Work? Targeting Meibomian Glands: Radiofrequency therapy targets the Meibomian glands, which are responsible for producing the oily layer of the tear film. In people with MGD, the oil produced by these glands can become thickened or clogged, leading to decreased oil production and an unstable tear film. This instability leads to dryness and increased evaporation of tears. Heat Application: The device used in RF therapy applies gentle heat to the eyelids using radiofrequency waves. The heat helps melt thickened meibum, clearing blockages in the glands. The heat also stimulates the glands, which can lead to increased production of normal, less viscous oils. Stimulation of Gland Function: The RF energy helps to enhance the natural function of the Meibomian glands, promoting healthier and more efficient oil production. This reduces the likelihood of blockages and helps to restore the tear film's lipid layer, which reduces tear evaporation and improves overall eye lubrication. Non-Invasive and Comfortable: RF therapy is a non-invasive procedure that does not involve direct manipulation of the glands, unlike manual gland expression. The process is generally comfortable, with patients often reporting a warm sensation on their eyelids during the treatment. Benefits of Radiofrequency Therapy for Dry Eye: Improves Meibomian Gland Function: RF therapy is particularly beneficial for people with Meibomian Gland Dysfunction (MGD), as it helps restore normal function to the glands, improves oil secretion, and enhances the overall tear film quality. Reduces Dry Eye Symptoms: By improving the quality and stability of the tear film, RF therapy can significantly reduce common dry eye symptoms such as dryness, itching, burning, and redness. The increased oil production helps reduce tear evaporation and provides better lubrication to the eye surface. Stimulates Collagen Production: Radiofrequency therapy can also stimulate collagen production in the eyelid tissues, which helps improve the structural integrity of the glands and surrounding tissues, potentially improving gland function over the long term. Safe and Non-Surgical: Unlike surgical options or invasive procedures, radiofrequency therapy is a non-surgical and non-invasive treatment that can be performed in an outpatient setting, making it a more accessible and less risky treatment option for those suffering from MGD-related dry eye. Minimal Downtime: There is minimal downtime after the procedure, with most patients experiencing little to no discomfort and being able to resume their normal activities immediately following treatment. Long-Lasting Relief: Many patients experience long-lasting improvement in symptoms following RF therapy, especially when combined with other dry eye treatments such as lid hygiene, lubricating eye drops, or omega-3 supplements. The Procedure: Pre-Treatment Preparation: Before the procedure, your eye care provider will assess your dry eye condition and may recommend a lid hygiene regimen to prepare the eyelids. Some topical anesthetic drops may be applied to ensure comfort during the treatment. Application of RF Energy: A specialized RF device is gently placed over the closed eyelids. The device generates radiofrequency energy that is delivered to the eyelid tissues. The heat generated by this energy will typically feel warm, and the provider will adjust the temperature and intensity for optimal comfort and effectiveness. Treatment Duration: Each session typically lasts between 15 to 20 minutes, depending on the severity of the dry eye and the area being treated. The treatment is typically well-tolerated, with minimal discomfort. Post-Treatment Care: After treatment, you may be advised to apply lubricating eye drops to help soothe the eyes. It’s important to avoid rubbing the eyes for a short period after the treatment to prevent irritation. Follow-up Treatments: Depending on the severity of your MGD and dry eye, you may need multiple treatments to achieve the desired results. Your eye care professional will tailor the treatment plan based on your specific needs. Side Effects and Considerations: Mild Discomfort: Some patients may experience mild discomfort or warmth during the procedure, but these sensations are typically brief and well-tolerated. Temporary Redness: After treatment, some people may notice mild redness or swelling of the eyelids, but this usually resolves quickly within a few hours. Sensitivity: A few individuals may experience temporary sensitivity to light or some irritation following the procedure, but these side effects are generally short-lived. Infection Risk: As with any eye treatment, it is important to follow aftercare instructions to reduce the risk of infection. However, RF therapy itself is low-risk when performed by a trained professional. Conclusion: Radiofrequency therapy is an effective, non-invasive treatment option for dry eye disease, particularly in cases where Meibomian Gland Dysfunction (MGD) is the primary cause. By applying gentle heat to the eyelid tissues, RF therapy helps unclog Meibomian glands, improve oil secretion, and restore tear film stability, leading to relief from common dry eye symptoms. It is a safe and well-tolerated treatment with minimal downtime and can be combined with other therapies for optimal results. Always consult with your eye care provider to determine if RF therapy is the right treatment option for you.
-
Thermal PulsationThermal Pulsation is a therapy in which the eyelids are heated and massaged to unclog oil glands. While this treatment is effective to relieve symptoms, we do not currently offer it as an option, as it does not treat the underlying cause. WHY are the oil glands clogged? Are they clogged because of low omega levels? Hormone imbalances? Rosacea, demodex mites, bacterial infections, poor blink, inflammation... We treat the underlying cause, not the symptom. We do not discount the fact that many patients feel a benefit from this treatment and will recommend an office who offers this procedure if we feel it would benefit you.
-
What Are Scleral LensesScleral lenses are a type of specialized contact lens that are larger than traditional contact lenses and designed to rest on the sclera (the white part of the eye), rather than directly on the cornea. These lenses are primarily used for people with irregular corneas, severe dry eye, and other complex visual or eye health issues that cannot be managed with standard contact lenses or glasses. Key Characteristics of Scleral Lenses: Large Diameter: Scleral lenses have a larger diameter than traditional soft contact lenses. While standard contact lenses typically measure 9-15 millimeters in diameter, scleral lenses usually range from 14 to 24 millimeters. They are large enough to vault over the cornea and rest on the sclera, creating a fluid reservoir between the lens and the eye. Gas Permeable Material: Scleral lenses are made of a rigid gas permeable (GP) material, meaning they allow oxygen to pass through the lens to the cornea, ensuring healthy oxygenation of the eye. This is in contrast to traditional soft contact lenses, which do not always allow as much oxygen to reach the eye. Comfort and Stability: The lenses are designed to be highly stable and comfortable, offering consistent vision correction. The larger size helps to keep the lens in place, and the rigid nature provides sharp, clear vision, especially for individuals with irregular corneas. Tear Reservoir: One of the key benefits of scleral lenses is that they create a tear reservoir between the lens and the cornea. The fluid beneath the lens can provide lubrication and hydration, which is especially beneficial for those with dry eye disease, meibomian gland dysfunction (MGD), or keratoconus. How Scleral Lenses Work: Vaulting Over the Cornea: Scleral lenses are designed to vault or "sit over" the cornea, creating a sealed chamber that is filled with a special saline solution (or sometimes lubricating drops). This reservoir of liquid helps to hydrate the cornea, providing relief from dry eye symptoms by keeping the eye moist and protected from environmental irritants. Providing Stable Vision: The rigid nature of scleral lenses helps to correct irregular corneas by creating a smooth optical surface. For people with conditions like keratoconus or corneal scars, these lenses improve vision clarity by compensating for the irregular shape of the cornea. Protecting the Ocular Surface: The lens acts as a shield over the cornea, which helps protect it from exposure to allergens, dust, wind, and other environmental factors that can exacerbate dry eye symptoms. It also minimizes irritation caused by blinking or excessive tear evaporation. Who Benefits from Scleral Lenses? Scleral lenses are especially helpful for individuals who suffer from complex eye conditions that cause either poor vision or discomfort. Some common conditions that benefit from scleral lenses include: Dry Eye Disease: Especially those with aqueous deficient dry eye or severe meibomian gland dysfunction (MGD). The lens provides a stable tear reservoir, helping to relieve discomfort associated with dry eye. Keratoconus: A condition where the cornea becomes thin and cone-shaped. Scleral lenses help provide clear vision by smoothing out the irregular surface of the cornea. Post-Surgical Conditions: After eye surgeries like LASIK or cataract surgery, scleral lenses can be used to protect the cornea and improve comfort if dry eye or scarring occurs. Corneal Scarring: If scarring is present due to injury or disease, scleral lenses can create a smooth surface for better vision and can help alleviate discomfort caused by the irregular corneal surface. Astigmatism: Severe astigmatism or irregular corneal shapes that cannot be fully corrected with regular contact lenses can benefit from the stability and vision clarity offered by scleral lenses. Sensitive Eyes: For individuals with highly sensitive eyes, scleral lenses can offer comfort by creating a cushion of moisture between the lens and the eye, protecting from dryness and irritation. Advantages of Scleral Lenses: Improved Comfort: Since they provide hydration and a stable tear film, scleral lenses can be more comfortable for people with dry eyes or other ocular surface diseases than traditional contact lenses. Clearer Vision: They can provide sharp, clear vision for people with irregular corneas or those who have not had success with traditional glasses or contact lenses. Protection for the Cornea: The lenses protect the cornea from exposure to irritants, environmental elements, and even physical trauma (like rubbing the eyes). Longer Wear Time: Due to the tear reservoir, scleral lenses can be worn for longer periods without causing discomfort or dryness compared to standard contact lenses. Customizable Fit: Scleral lenses are custom-made to fit the unique shape of the patient's eye, ensuring better comfort and effectiveness than standard lenses. Potential Drawbacks: Fitting Process: Fitting scleral lenses requires a specialized fitting process and may take longer than traditional contact lenses. Multiple visits may be needed to ensure the lens is providing the best fit and comfort. Maintenance: Scleral lenses require more care and cleaning than regular contact lenses. They need to be disinfected properly and the tear reservoir must be filled with sterile saline or other recommended solutions. Cost: Scleral lenses tend to be more expensive than traditional lenses, due to the custom fitting process and specialized materials used. However, many patients find the benefits to be well worth the cost. Learning Curve: New users may experience a learning curve when it comes to inserting and removing scleral lenses. The process requires some practice and care, especially given the lens's large size. Conclusion: Scleral lenses are a highly effective treatment option for individuals with complex eye conditions like severe dry eye disease, keratoconus, and post-surgical recovery. They offer both vision correction and comfort by creating a tear reservoir between the lens and the eye, providing hydration and protection to the cornea. While they require a specialized fitting process and ongoing care, scleral lenses can significantly improve the quality of life for those with difficult-to-manage eye conditions. If you're considering scleral lenses, consult an eye care professional who specializes in contact lenses for a proper fitting and to determine if they are the right option for you.add description
-
My Lenses are Fogging, What Can I Do?Midday fogging is a common issue for scleral lens wearers and refers to a feeling of blurry or hazy vision that typically occurs in the afternoon or mid-day, even after the lens has been properly fitted and initially feels comfortable. This can be frustrating because it impacts the clarity of vision, especially since scleral lenses are designed to provide stable and clear vision throughout the day. Causes of Midday Fogging in Scleral Lenses: Lens Deposits: Over time, proteins, lipids, and other debris from tears can accumulate on the surface of the lens. This can lead to a build-up that clogs the lens or makes it harder to maintain a clear, smooth surface. The foggy feeling is a result of light scattering due to these deposits on the lens. Dryness or Evaporation: While scleral lenses are designed to create a tear reservoir between the lens and the cornea, over the course of the day, the moisture in the reservoir can evaporate. As the tear film evaporates, the lens may start to dry out, leading to discomfort and visual blurring. This is particularly common in dry environments or for people with aqueous deficient dry eye. Incomplete Tear Reservoir: Sometimes the tear reservoir doesn’t fully fill due to improper lens fit, lens misalignment, or insufficient tear production. This can cause the lens to interact directly with the cornea, which results in blurry or foggy vision. Increased Tear Viscosity: As the day progresses, the tear film may become thicker or more viscous, especially if you're not blinking as frequently or are in a dry environment. This can lead to fogging and reduced clarity of vision. Contact Lens Movement: If your scleral lenses move or shift slightly throughout the day, the reservoir between the lens and the cornea may disturb the tear film, causing fogging. This is often more noticeable if the lenses are not perfectly centered or are slightly too large or small. Lens or Eye Surface Contamination: Small particles, dust, or even allergens can get trapped between the scleral lens and the cornea, causing a foggy sensation. This can occur especially in windy or dusty environments. What You Can Do to Prevent or Resolve Midday Fogging: Proper Lens Cleaning: Ensure that your scleral lenses are thoroughly cleaned and disinfected after each use to prevent the buildup of deposits on the lens surface. Use the recommended cleaning solutions, such as Boston Simplus (for gas permeable lenses) or other solutions that help remove protein deposits. Soaking the lenses overnight in a cleaning solution can help maintain the smooth surface of the lens and minimize fogging. Lubricating Drops: Use preservative-free lubricating drops designed for scleral lenses throughout the day. These drops can help replenish the tear reservoir under the lens and improve clarity. Add moisture to the tear film by applying drops directly to the lens surface or the eye during the day to prevent drying and fogging. Check for Proper Fit: Ensure that your scleral lenses fit properly. If they are too tight or too loose, they may not create an adequate tear reservoir, leading to fogging. Your optometrist or ophthalmologist should monitor the fit to ensure the lens sits comfortably and appropriately on your eye. Proper alignment of the lens is also important—if the lens isn’t centered, the tear reservoir might not fill evenly, contributing to fogging. Use of a Cleaning or Rewetting Solution: Rewetting solutions specifically for scleral lenses can be used to refresh the tear film and help reduce fogging. Some solutions are designed to help with moisture retention throughout the day. Blinking More Often: Frequent blinking can help ensure the lens moves slightly and that the tear film beneath the lens remains distributed evenly. Blinking also helps keep the eyes hydrated, so consider consciously increasing your blink rate, especially if you're concentrating on a screen or have been in a dry environment. Avoid Dry or Irritating Environments: Try to avoid or minimize time spent in dry environments, such as air-conditioned rooms or windy conditions, as this can increase evaporation and exacerbate dryness. If you're in a dry environment, consider using a humidifier to help maintain moisture in the air, or wear protective eyewear to reduce exposure to wind or air drafts. Ensure Adequate Tear Film Production: If you have aqueous deficient dry eye, talk to your eye care professional about other treatments, such as punctal plugs, anti-inflammatory medications, or preservative-free artificial tears that can help improve tear production. You might need additional treatment to support adequate tear production throughout the day. Avoid Touching the Lenses: Avoid touching your lenses during the day if you can. Fingerprints or dirt on the lenses can cause fogging. If necessary, use a clean tissue to gently clean the lens. Monitor Your Diet and Hydration: Staying well-hydrated can help maintain a stable tear film. Dehydration can contribute to dry eyes, leading to lens fogging. Additionally, consider foods rich in omega-3 fatty acids, such as fish or flaxseed, as they may help improve tear production. When to See an Eye Care Professional: If midday fogging persists despite trying the above strategies, it's important to consult with your optometrist. They may recommend: Reevaluating the fit of your scleral lenses. Checking for underlying conditions like dry eye disease or meibomian gland dysfunction (MGD) that might be contributing to the fogging. Adjusting your prescribed lens materials or the lens design (e.g., a different curvature or diameter). Persistent fogging could also indicate that there is a more complex issue with your scleral lenses or your ocular health, requiring professional evaluation and care. Conclusion: Midday fogging in scleral lens wearers can be caused by factors like lens deposits, dryness, evaporation, or an improper fit. To address this issue, maintaining proper lens hygiene, using lubricating drops, ensuring a proper fit, and minimizing environmental factors can help prevent and alleviate the problem. If these measures don’t resolve the issue, seeking guidance from your eye care professional is important for finding a tailored solution.
-
How do I travel with scleral lenses?Dr. McConkey provides all scleral lens patients with a TSA Letter of Medical Necessity. To prepare for your trip, follow the tips below: Traveling with scleral lenses through TSA (Transportation Security Administration) can be a smooth process if you're well-prepared. Here are some tips to help ensure that you travel with your lenses safely and without any issues: 1. Carry Your Scleral Lenses and Solutions in the Correct Containers Lens Case: Always bring a clean, empty lens case to store your lenses while traveling. It’s a good idea to bring extra lens cases in case of any issues. Saline Solution: When carrying ScleralFil saline or any other solutions (such as disinfecting or storing solution like Boston Simplus), make sure the containers are 3.4 ounces (100 milliliters) or smaller. This is the TSA regulation for liquids in carry-on bags. All liquids must be placed in a quart-sized bag and be easily accessible during screening. Keep Solution and Lenses in Original Packaging: If possible, keep your saline solution and cleaning solutions in their original packaging to make them more easily identifiable during security screening. 2. TSA’s 3-1-1 Rule for Liquids 3-1-1 Rule: TSA’s liquid rule allows only 3.4 ounces (100 ml) per container of liquid, gel, or aerosol. All containers must fit into a single 1 quart-sized clear plastic bag. Each passenger is allowed one quart-sized bag. Medically Necessary Items: Scleral lenses and their associated solutions are considered medically necessary items. You are allowed to carry larger quantities of saline or cleaning solutions beyond the 3.4-ounce limit, as long as they are medically necessary. However, you will need to inform the TSA officer about this before you go through security. 3. Declare Your Items at Security When you reach the security checkpoint, inform the TSA officer that you are carrying scleral lenses and their solutions. It's best to declare it upfront to avoid any confusion or delays. You may be asked to remove the saline bottles and any other liquid items from your bag and place them separately for inspection, especially if they exceed the standard 3.4-ounce limit. TSA officers are usually familiar with medical supplies like scleral lenses, but it can help to be prepared with any documentation or a doctor's note, just in case. 4. Consider Using a Travel Lens Kit If you need to carry more solution, consider using a travel lens kit designed for convenience and to hold extra solutions and accessories in a compact manner. Some kits come with mini bottles that are TSA-friendly or include a cleaning system specifically for travel. Make sure all liquids are properly labeled and meet TSA’s liquid restrictions. 5. Bring Extra Lenses Always bring extra scleral lenses (at least one pair) in case of any issues during travel. Keep them in their own sealed case to prevent contamination. It’s a good idea to keep the spare lenses in your carry-on bag, as checked luggage can sometimes experience delays or mishandling. 6. Keep Your Lenses Comfortable While Traveling Lubricating Drops: Consider bringing preservative-free lubricating drops or artificial tears in your carry-on bag, especially if your eyes tend to get dry during travel. Again, these drops should comply with the TSA 3-1-1 liquid rules. Hydration: Air travel can dry out your eyes, so staying hydrated with water during the flight will help maintain comfort when wearing your lenses. 7. Screening Process Security Screening: When going through the security scanner, you can leave your scleral lenses and solutions in your carry-on bag, but be prepared for additional screening if required. X-ray machines are generally safe for lenses and solutions. Pat-Down or Additional Screening: In rare cases, TSA officers may request a pat-down or additional inspection of your items. This is typically because of medical devices or liquids that exceed the usual limit. 8. Use Your Scleral Lenses During Travel (Optional) Some travelers prefer to wear their scleral lenses throughout the flight instead of carrying a backup pair. Just make sure you have your lens care products with you for the trip, and take your lenses out as needed for cleaning or if they become uncomfortable. 9. Be Prepared for Any TSA Questions TSA agents may ask about your lenses and solutions, so it’s helpful to know the details of your lens care regimen (e.g., the saline solution and cleaning system you use). You don’t need a doctor’s note unless you’re carrying larger-than-usual amounts of solution or if you're traveling internationally. However, if you're concerned, you can always request one from your eye care provider as an extra precaution. 10. Traveling Internationally If you’re flying internationally, check the regulations of the country you’re traveling to, as some countries may have different restrictions for medical supplies and liquids. In Summary: To travel smoothly with scleral lenses through TSA: Keep your saline solution and lens care products within the 3.4-ounce (100 ml) rule for liquids. Inform the TSA officer that you're carrying medically necessary items. Store the lenses in their lens case and keep them accessible. Consider carrying extra lenses and lens care supplies for peace of mind. Use lubricating eye drops to keep your eyes comfortable during the flight. Being prepared and understanding TSA’s regulations will make your travel experience with scleral lenses easier and more convenient.
-
How do I care for my scleral lenses?Materials Needed: Scleral contact lenses Boston Simplus Solution (for cleaning, disinfecting, and storing) Scleralfil Saline Solution (for rinsing and filling lenses) Lens case Clean towel or paper towel (for drying) Daily Care and Cleaning Routine Wash Your Hands: Before touching your contact lenses, thoroughly wash your hands with lotion free soap and water. Dry them with a clean, lint-free towel. Remove the Scleral Lenses: Carefully remove your scleral lenses from your eyes using the recommended technique provided by your eye care professional. Always make sure your fingers are clean and dry to prevent contamination of the lenses. Clean the Lenses with Boston Simplus: Place the lens in the palm of your hand. Add 2-3 drops of Boston Simplus solution onto the lens. Gently rub the lens with your fingertip for about 10-15 seconds on each side to help remove any debris or buildup. After rubbing the lenses, rinse both sides of the lens with Boston Simplus to remove any residual solution or contaminants. Disinfect the Lenses: After cleaning, place the lenses in your clean lens case. Fill the case with fresh Boston Simplus solution, ensuring that the lenses are fully submerged. Leave the lenses in the solution for a minimum of 4 hours to allow for proper disinfection. Do not use tap water to clean or store your lenses. Always use the recommended solutions to prevent infection. Store the Lenses: Keep the lens case tightly closed when not in use. Store the case in a cool, dry place, and avoid exposure to heat or direct sunlight. Before Inserting Lenses (Rinsing and Filling) Wash Your Hands: Wash and dry your hands thoroughly before handling your lenses. Rinse the Lenses with Scleralfil Saline: Take the cleaned and disinfected scleral lens from the storage case. Rinse the lens with Scleralfil saline solution to remove any cleaning solution or debris. Use Scleralfil saline to fill the lens reservoir: Fill the lens with Scleralfil saline (the saline is designed for the large reservoir in scleral lenses). Hold the lens upright and slowly fill it until the reservoir is full. You can also place the saline directly into the lens as you prepare to insert it. Insert the Lenses: With the saline inside, gently insert the lens into your eye. Blink a few times to ensure the lens is comfortable and properly centered. Additional Tips: Always use fresh solution: Never reuse the solutions (either Boston Simplus or Scleralfil saline). Always discard any remaining solution after use. Keep the lens case clean: Clean your lens case daily by rinsing it with fresh Boston Simplus and allowing it to air dry. Never touch the lens surface: When handling the lenses, avoid touching the surface that will come into contact with your eye to prevent contamination. By following these instructions, you can ensure that your scleral lenses stay clean, comfortable, and safe to use. Always follow your eye care professional’s guidance for your specific needs. Here’s a list of helpful tips for using scleral contact lenses to ensure comfort, safety, and longevity: 1. Always Wash Your Hands: Before handling your lenses, wash your hands thoroughly with lotion free soap and water to prevent contamination and infections. 2. Use the Right Solutions: Boston Simplus is typically used for cleaning, disinfecting, and storing scleral lenses. Scleralfil saline should be used for rinsing the lenses before insertion and for filling the lens reservoir. 3. Clean Lenses Properly: Clean your lenses daily by rubbing them with cleaning solution (like Boston Simplus) for 10-15 seconds to remove any debris. Never use tap water to clean your lenses, as it can introduce harmful bacteria. 4. Store Lenses in Fresh Solution: Always store your lenses in fresh solution in a clean case. Avoid reusing old solution. Make sure the lenses are fully submerged in the solution to ensure proper disinfecting. 5. Inspect Lenses Before Inserting: Inspect each lens for any visible damage or debris before insertion. Look for any tears, cracks, or deposits. Ensure there are no air bubbles in the lens reservoir when inserting. 6. Rinse Lenses with Saline Before Insertion: Before putting lenses in your eyes, rinse them with Scleralfil saline to remove any residual cleaning solution and hydrate the lens. 7. Apply Scleral Lenses with Care: When inserting your lenses, use a gentle, steady hand. Hold your eyelids open and place the lens on the eye without force. If the lens feels uncomfortable, remove it and recheck for debris or improper insertion. 8. Keep Your Lens Case Clean: Clean your lens case every day with Boston Simplus solution and let it air dry. Replace your lens case every 1-3 months. 9. Avoid Sleeping in Lenses: Unless specifically prescribed, avoid wearing your scleral lenses overnight. Sleeping in lenses can increase the risk of infections and discomfort. 10. Stay Hydrated: Scleral lenses create a reservoir of saline between your eye and the lens. If your eyes feel dry or uncomfortable, ensure you are properly hydrating throughout the day. 11. Be Mindful of Lens Drying: Never let your lenses dry out completely. If they do, they could become damaged, making them difficult or uncomfortable to wear. 12. Follow Replacement Schedules: Scleral lenses have a recommended lifespan. Make sure to replace them according to your eye care professional's instructions. 13. Use a Lens Insertion and Removal Tool: If you find it difficult to handle the lenses with your fingers, consider using a lens inserter/remover tool. This can help avoid direct contact with your lenses and reduce the risk of contamination. 14. Monitor for Discomfort or Vision Changes: If you experience persistent discomfort, vision changes, or irritation, remove the lenses immediately and contact your eye care provider. 15. Do Not Share Your Lenses: Never share your scleral lenses with others, as this can lead to serious eye infections. 16. Regularly Visit Your Eye Care Professional: Schedule regular check-ups with your eye care professional to ensure the lenses fit properly, your eyes are healthy, and any issues are addressed promptly. By following these tips, you can maximize the comfort and safety of wearing scleral lenses, ensuring they provide the best vision correction while maintaining eye health.
-
What is Hydrapeg?More information coming soon
-
How often do I have to replace my scleral lenses?Scleral lenses should be replaced every 1 to 2 years, to prevent warpage, and possible complications. You should have your eyes examined at least once a year if you wear scleral lenses.
-
If My Eyes Are Dry, Why Do They Water?Watery eyes (epiphora) can occur when the eyes are dry due to several reasons, even though it may seem counterintuitive. This happens because the eye is trying to compensate for a lack of moisture or lubrication. Here’s why this occurs: 1. Reflex Tearing: When the eyes become dry, the body often responds by producing more tears in an attempt to protect and lubricate the eye. These are called reflex tears, and they are different from the normal tear film that keeps your eyes moist. Reflex tears are often more watery and less stable than normal tears, and they can flood the eye in an attempt to wash away irritants and alleviate dryness. 2. Inadequate Tear Film: In dry eye disease, the tear film that normally coats the surface of the eye is unstable. The tear film has three layers: a watery layer, an oily layer, and a mucous layer. When there’s a lack of aqueous (watery) component, the eye surface becomes irritated and dry. The brain detects the irritation and sends signals to the lacrimal glands to produce more tears, but they may not be of the correct consistency, leading to excessive watery tearing as the eye compensates. 3. Meibomian Gland Dysfunction (MGD): Meibomian glands are responsible for producing the oily layer of the tear film, which helps prevent tear evaporation. If these glands aren’t working properly (a condition called meibomian gland dysfunction or MGD), tears evaporate too quickly, and the eye becomes dry. In response, the eye may start producing more watery tears (reflex tears) to make up for the missing moisture, but these tears won’t be as effective in keeping the eye lubricated, leading to a cycle of dryness and excess tearing. 4. Blocked Tear Ducts: Tear drainage occurs through small openings in the eyelids called puncta. If the puncta become partially blocked or narrowed, tears can’t drain efficiently, leading to a buildup of excess tears on the surface of the eye, even if the eye is still dry. This can cause watery eyes, even when the tear production is inadequate. 5. Environmental Irritants: Dry conditions, such as wind, dry air, smoke, or air conditioning, can exacerbate dry eye symptoms. The eye may produce more tears as a response to irritation caused by environmental factors, but the tears produced may not adequately lubricate the eye, leaving it feeling both watery and dry. 6. Allergic Reactions: Allergies can also cause dryness and watering at the same time. In allergic reactions, the body releases histamines in response to allergens like pollen, dust, or pet dander. This causes inflammation and irritation of the eyes, leading to dry eye symptoms and an overproduction of watery tears as the body tries to flush out the irritants. 7. Medication Side Effects: Certain medications can cause both dryness and excessive tearing as side effects. Medications like antihistamines or diuretics can reduce tear production, leading to dryness, while other medications can trigger reflex tearing. 8. Age-related Changes: As people age, tear production decreases, and the quality of tears may worsen. This can lead to a sensation of dry eyes, causing the body to produce watery tears to compensate for the dryness. Summary: The combination of insufficient tear production, tear instability, and irritation is typically responsible for watery eyes in the context of dry eye disease. Your body attempts to compensate for the dryness by producing more tears, but these tears are often not of the right consistency, leading to watery eyes without sufficient lubrication. If you're experiencing this issue regularly, it might be a sign of dry eye disease or another underlying condition, and it may be worth consulting an eye care professional for diagnosis and treatment.
-
What causes dry eyes?Dry eye disease is a complex condition that can be caused by a variety of factors, many of which can work together to create or exacerbate symptoms. Below, we'll explore each of the causes you mentioned, along with how they contribute to dry eye: 1. Low Tear Production (Aqueous Deficiency) Cause: When the lacrimal glands (tear-producing glands) are not producing enough tears, the eye becomes dry and irritated. This can occur due to a reduced volume of tears or poor quality of the tears. Common Causes: Aging: Tear production naturally decreases with age, especially after the age of 50. Autoimmune diseases: Conditions like Sjögren’s syndrome, Rheumatoid arthritis, and lupus can damage the tear-producing glands, leading to insufficient tear production. Medications: Certain medications (e.g., antihistamines, antidepressants, diuretics, and beta-blockers) can reduce tear production. Environmental factors: Dry, windy, or smoky environments increase the evaporation of tears and can contribute to dry eye. 2. Meibomian Gland Dysfunction (MGD) Cause: The Meibomian glands, located in the eyelids, secrete an oily substance that forms the lipid layer of the tear film, which helps to prevent tear evaporation. When these glands are blocked or dysfunctional, they do not produce enough oil, and tears evaporate too quickly. Common Causes: Aging: Meibomian gland function declines with age. Blepharitis: Inflammation of the eyelids, often due to bacteria or poor hygiene, can block the Meibomian glands. Environmental factors: Dry air, wind, and extended screen time can aggravate MGD. Hormonal imbalances: Changes in hormones (e.g., during menopause) can reduce the function of the Meibomian glands, leading to dry eye. Systemic conditions: Rosacea, diabetes, and hyperthyroidism can contribute to MGD. 3. Incomplete Blink Cause: The act of blinking is essential for spreading the tear film evenly across the eye. If blinking is incomplete or infrequent, the tear film may not be distributed properly, leaving the eye surface exposed to environmental irritants. Common Causes: Prolonged screen time: Staring at digital screens (computers, phones, etc.) leads to reduced blink rate. People typically blink less frequently when looking at screens. Fatigue or stress: Being tired or anxious can lead to shallow and incomplete blinking. Neurological conditions: Diseases like Parkinson's disease or Bell’s palsy can affect the muscles controlling the eyelids and lead to incomplete blinking. 4. Low Omega-3 Fatty Acids Cause: Omega-3 fatty acids play an important role in the quality of the lipid layer of the tear film, produced by the Meibomian glands. Omega-3s have anti-inflammatory properties and can help reduce the thickness of the oils produced by the Meibomian glands, allowing them to function more effectively. Common Causes: Dietary deficiencies: A diet low in omega-3 fatty acids (found in fish like salmon, flaxseeds, walnuts, and chia seeds) can affect tear film stability. Inflammation: Inflammatory conditions, such as MGD or autoimmune diseases, can reduce the beneficial effects of omega-3s on the eyes. 5. Autoimmune Diseases Cause: In autoimmune diseases, the body’s immune system attacks its own tissues, including those that produce tears. This can significantly affect both tear production and the quality of the tear film. Common Autoimmune Diseases: Sjögren’s syndrome: A condition where the immune system attacks the lacrimal and salivary glands, leading to severely reduced tear production. Rheumatoid arthritis: An inflammatory condition that can also impact tear production and Meibomian gland function. Lupus: An autoimmune disease that can cause inflammation in the eye glands, leading to dry eye. 6. Hormonal Imbalances Cause: Hormonal changes can have a significant impact on dry eye. Estrogen and progesterone can influence the function of the lacrimal glands and Meibomian glands, particularly in women. Common Causes: Menopause: A significant drop in estrogen during menopause can lead to decreased tear production and Meibomian gland dysfunction. Pregnancy and birth control: Hormonal fluctuations during pregnancy or as a result of birth control can also affect tear production. 7. Incomplete Lid Closure Cause: When the eyelids do not fully close during blinking or while sleeping, the tear film can evaporate too quickly, leading to dry eye. Common Causes: Eyelid abnormalities: Conditions like ptosis (drooping eyelids) or entropion (inward-turning eyelids) can prevent full closure. Neurological conditions: Bell’s palsy or other conditions affecting the facial muscles can impair eyelid closure. Contact lens wear: Extended wear of contact lenses, especially hard or scleral lenses, can lead to incomplete closure during sleep. 8. Allergies Cause: Allergic reactions can cause inflammation and irritation of the eyes, leading to dry eye symptoms. Allergies can cause the eyes to become more sensitive to environmental factors, making them more susceptible to dryness and discomfort. Common Causes: Pollen, dust, pet dander: These common allergens can trigger inflammation and worsen dry eye symptoms. Medication: Some allergy medications (especially antihistamines) can reduce tear production and contribute to dry eye. 9. Contact Lens Wear Cause: Contact lenses can exacerbate dry eye in several ways. The lenses can interfere with the normal tear exchange on the eye surface, lead to a decrease in oxygen supply to the cornea, and increase the evaporation of tears. Common Causes: Extended wear: Wearing contact lenses for extended periods (especially overnight) can cause the eyes to dry out. Lens material: Some contact lenses (particularly rigid lenses or older types of soft lenses) may not allow for proper tear exchange, leading to dryness. Lens hygiene: Inadequate cleaning or improper handling of lenses can lead to irritation and dryness. 10. History of LASIK Surgery Cause: LASIK (Laser-Assisted In Situ Keratomileusis) is a surgical procedure that reshapes the cornea to correct refractive errors. However, one of the potential side effects is the development of dry eye, due to the surgery affecting the corneal nerves, which play a key role in tear production and blink reflex. Common Causes: Reduced corneal sensation: After LASIK, the nerves responsible for triggering tear production may be temporarily or permanently reduced. Post-operative inflammation: Inflammation after surgery can lead to a decrease in tear production and exacerbate dry eye symptoms. 11. Medications Cause: Many medications can contribute to dry eye by reducing tear production or causing inflammation of the eye. Common Medications: Antihistamines: Commonly used for allergies, antihistamines can reduce tear production. Antidepressants: SSRIs, SNRIs, and other antidepressants can cause dry eye as a side effect. Diuretics: Often used for high blood pressure, diuretics can lead to dehydration, which can reduce tear production. Beta-blockers: These medications, commonly prescribed for heart conditions or high blood pressure, can also reduce tear production. Hormonal treatments: Birth control pills, hormone replacement therapy (HRT), and some other hormonal medications can alter tear production and exacerbate dry eye symptoms. Summary of Contributing Factors: Low tear production (due to aging, autoimmune disease, medications, environmental factors). Meibomian gland dysfunction (MGD) (caused by inflammation, aging, hormonal changes, and systemic conditions). Incomplete blinking (due to screen time, fatigue, neurological conditions). Low omega-3 levels (due to dietary deficiencies, inflammation, or MGD). Autoimmune diseases (like Sjögren’s syndrome, rheumatoid arthritis). Hormonal imbalances (especially during menopause, pregnancy, or use of hormonal medications). Incomplete lid closure (due to eyelid abnormalities, neurological conditions, or contact lens wear). Allergies (causing eye inflammation and irritation). Contact lens wear (especially extended wear or improper lens care). History of LASIK (which may reduce corneal sensation and affect tear production). Medications (such as antihistamines, antidepressants, diuretics, and beta-blockers). Each of these factors can either cause or contribute to dry eye by impairing the production, quality, or stability of the tear film. Often, multiple factors interact to cause or worsen symptoms. Treatment typically focuses on addressing the underlying cause(s) and may involve a combination of artificial tears, prescription medications, lifestyle changes, and in some cases, surgical interventions. Consulting with an eye care professional is essential for identifying the specific causes and tailoring an effective treatment plan.
-
Can dry eye cause blurred vision?Yes, dry eye disease can cause blurred vision, and this is a common symptom experienced by individuals with the condition. Here’s how it happens: 1. Tear Film Instability The tear film that covers the surface of the eye is essential for clear vision. When the tear film is unstable due to insufficient tears or poor-quality tears (as is often the case in dry eye disease), the vision can become blurry. Dry spots on the cornea (the clear, front surface of the eye) may form when the tear film breaks down, leading to intermittent or persistent blurred vision. The blurriness can improve or change throughout the day as the tear film fluctuates. 2. Fluctuating Vision People with dry eyes often experience fluctuating or intermittent blurred vision. This is due to the uneven spread of the tear film across the corneal surface, causing variations in vision clarity. Blurring may worsen in dry environments or after prolonged screen time, as the tear film can evaporate more quickly in these situations. 3. Meibomian Gland Dysfunction (MGD) A common cause of dry eye is Meibomian gland dysfunction (MGD), where the glands that produce the oily layer of the tear film are blocked or produce insufficient oil. This leads to an unstable lipid layer, causing increased tear evaporation. The lack of proper tear lubrication can result in blurry vision that can be temporarily improved after blinking or applying artificial tears. 4. Inflammation and Surface Damage Chronic dryness can lead to inflammation on the surface of the eye, further disrupting the tear film and contributing to blurred vision. In some cases, abrasions or microdamage to the corneal surface (from dryness or incomplete blinking) can worsen the blurriness. 5. Contact Lens Wear For contact lens wearers, dry eye can cause lens discomfort, which can lead to blurred vision. The lenses may not move smoothly over the eye, causing inconsistent vision or dryness under the lens. 6. Medication Side Effects Certain medications used to treat dry eye (like anti-inflammatory eye drops) or other conditions can have side effects that cause temporary blurred vision as a result of dryness or the properties of the medication. 7. Fluctuation with Time of Day Dry eye symptoms, including blurred vision, often worsen as the day progresses due to tear evaporation and reduced tear production over time. This may result in clearer vision in the morning (after a night of rest and tear replenishment) and blurrier vision as the day goes on. If you are experiencing persistent blurred vision due to dry eye, it’s important to consult with an eye care professional to determine the cause and receive appropriate treatment. It is not recommended to update your glasses or contact lens prescription until your dry eye is controlled.
-
What lifestyle modifications can help dry eye?Lifestyle changes can play a significant role in managing dry eye disease (DED) and improving overall eye comfort. Here are several lifestyle modifications that can help reduce symptoms and improve the health of your eyes: 1. Maintain Proper Hydration Drink plenty of water throughout the day to stay hydrated. Dehydration can contribute to reduced tear production and worsen dry eye symptoms. Aim for at least 8 glasses of water daily, but your needs may vary depending on activity level, climate, and overall health. 2. Use Humidifiers Increase humidity in dry environments by using a humidifier in your home, especially during winter when indoor heating can dry out the air. Humidifiers can help prevent the evaporation of tears and improve overall eye comfort. 3. Adjust Your Environment Avoid direct air flow from fans, air conditioning, or heaters that can dry out the eyes. Position yourself away from windy or dry conditions when possible, as environmental factors like wind, smoke, and low humidity can exacerbate dry eye. 4. Practice the 20-20-20 Rule for Screen Time Take regular breaks from digital screens. Every 20 minutes, look at something 20 feet away for at least 20 seconds. This helps reduce eye strain and encourages natural blinking. Consider using screen filters or apps that reduce blue light exposure, which can further irritate the eyes. 5. Increase Omega-3 Fatty Acids Incorporate omega-3 fatty acids into your diet to help improve the quality of your tear film. Omega-3s can be found in fatty fish (like salmon, mackerel, and sardines), flaxseeds, chia seeds, and walnuts. Omega-3 supplements (fish oil or flaxseed oil) can also be taken if you do not consume enough omega-3s through diet alone. 6. Use Artificial Tears Regularly Lubricating eye drops can help keep your eyes moist and reduce irritation. Use preservative-free drops if you need to apply them frequently to avoid irritation. Consider using gel-based or ointment-style drops at night for longer-lasting relief. 7. Practice Proper Lid Hygiene Clean your eyelids and lashes regularly to reduce inflammation and prevent conditions like blepharitis and meibomian gland dysfunction (MGD). You can use eyelid wipes or a gentle eyelid cleanser to remove debris and oil buildup. Warm compresses followed by lid massage can help unclog the Meibomian glands and improve oil flow, which helps stabilize the tear film. 8. Wear Protective Eyewear Sunglasses or goggles can protect your eyes from wind, dust, and harmful UV rays when outdoors. Choose sunglasses with wraparound frames to reduce exposure to environmental factors. Consider wearing moisture chamber glasses that create a small, humidified environment around your eyes, which can help prevent tears from evaporating quickly. 9. Blink More Frequently Make a conscious effort to blink more often, especially during tasks that require focus (like reading or using a computer). Blinking helps distribute the tear film evenly across the eye's surface. Exercise your eyelids to help encourage full, complete blinks. 10. Modify Your Diet Avoid foods that can increase inflammation: Try to limit the intake of processed foods, sugary snacks, and refined carbohydrates, which can contribute to inflammation. Incorporate anti-inflammatory foods: Foods like leafy greens, berries, nuts, and olive oil may help reduce inflammation and promote overall eye health. 11. Manage Allergies Control allergies with proper medication or lifestyle changes. If you have seasonal allergies, try to reduce exposure to allergens (e.g., pollen, dust) and manage symptoms with antihistamines, allergy eye drops, or nasal sprays. Keep windows closed during high pollen seasons and consider using air purifiers in your home to reduce airborne allergens. 12. Take Care of Your Sleep Get enough sleep each night (typically 7-9 hours) to allow your eyes to fully rest and replenish their natural moisture. Consider using moisture-retaining sleep masks if you experience dryness overnight or have issues with incomplete lid closure during sleep (a condition called nocturnal lagophthalmos). 13. Exercise Regularly Exercise can help improve circulation, which in turn may promote overall eye health. Regular physical activity can also help reduce inflammation in the body, which may benefit people with dry eye related to systemic conditions like autoimmune disease. 14. Limit or Avoid Smoking Smoking can increase dry eye symptoms by reducing tear production and increasing inflammation in the eyes. It also exposes the eyes to harmful chemicals that can worsen eye irritation. Avoid secondhand smoke as well, as it can have similar effects on the eyes. 15. Optimize Contact Lens Wear and Care If you wear contact lenses, follow proper cleaning and maintenance instructions to avoid irritation and infection. Consider switching to scleral lenses or soft lenses designed for dry eye if traditional lenses worsen symptoms. Take breaks from contact lens wear to allow your eyes to breathe and reduce the risk of dryness. 16. Follow Up with Your Eye Doctor Regularly visit your eye care professional for check-ups, especially if you have underlying conditions (like autoimmune diseases or Meibomian gland dysfunction) that affect dry eye. Your doctor may recommend specific treatments, such as punctal plugs or prescription eye drops, based on your individual condition. 17. Consider Stress Management Chronic stress can exacerbate inflammation and worsen dry eye symptoms. Practice relaxation techniques like deep breathing, yoga, or meditation to help reduce stress levels and improve overall eye comfort. 18. Reduce Use of Harsh Medications If possible, work with your healthcare provider to adjust medications that may contribute to dry eye symptoms. Medications like antihistamines, antidepressants, and diuretics can reduce tear production. Your doctor may be able to adjust the dosage or suggest alternative treatments. Conclusion: Incorporating these lifestyle changes can help manage dry eye disease, reduce discomfort, and improve the overall health of your eyes. Maintaining hydration, improving environmental conditions, practicing good eye hygiene, and modifying your diet can all contribute to better tear production and stability. It’s important to remember that dry eye disease is multifactorial, so a combination of strategies may be necessary to effectively manage symptoms. Always consult your eye care provider to determine the best approach for your specific condition.
-
Why was I told my eyes are dry, even though they don't feel dry?Not all dry eyes feel dry. Patients who have tears that evaporate too quickly, causing a reflex to produce more tears. In this case, the tears are not good quality, and result in excessive tearing. Other causes of eyes not feeling dry include losing corneal sensation due to the trauma caused by dry eye, corneal surgeries, and other insults to the corneal nerves. This is called neurotrophic keratitis.
-
Why was my prescription sent to a specialty pharmacy?Insurance companies are complicated and will deny dry eye medications frequently. To combat this, we work with pharmacies who have partnered with drug companies, to reduce the cost to patients. It is not unusual for Dr. McConkey to prescribe a medication that gets denied by your insurance company. In many cases, we will fill out a prior authorization. In some cases, this prior authorization is also denied. When this happens, specialty pharmacies will give patients a reduced price on their medications, make it much more affordable than sending to a local pharmacy. Not all medications are created equal, and to provide you with the best care possible, we may encourage you to use brand name medications over generic when appropriate. If you have questions regarding any of these pharmacies, please contact our office for further information. *Note, not all patients will be able to utilize specialty pharmacies. In this case, we will send to your local pharmacy. To help us get your drugs covered faster, it is beneficial if you provide us with your Prescription Drug Formulary.
-
Why do my eye drops burn?Dry eye causes inflammation and tissue damage to the front of the eye. Many drops we prescribe will burn due to the "water on fire" effect. Over the course of about three months, these symptoms should improve, as the anti-inflammatory drops reduce inflammation, there will be less of a reaction. Additionally, tissue damage from dry eye causes exposed nerve endings, which will cause many drops to be uncomfortable, until the eye heals. Please be patient, but also inform our office if you are unable to tolerate your eye drops.
-
RestasisRestasis (generic name: cyclosporine) is a prescription eye drop medication used to treat chronic dry eye disease (DED), a condition where the eyes don’t produce enough tears or the tears evaporate too quickly, causing irritation, inflammation, and discomfort. Restasis is specifically designed to help increase the production of natural tears in individuals whose dry eye disease is caused by inflammation. How Restasis Works: Restasis is an immunosuppressant medication that works by targeting and reducing the inflammation in the tear-producing glands (lacrimal glands). It does this by inhibiting the activity of certain immune cells that contribute to inflammation. This helps improve tear production and reduce the symptoms of dry eyes. Unlike lubricating eye drops that temporarily relieve symptoms of dry eye, Restasis works by addressing the underlying inflammation to help the eyes produce more of their natural tears over time. How to Use Restasis: Restasis is usually prescribed as one drop in each eye twice a day, about 12 hours apart. Possible Side Effects: Like all medications, Restasis can cause side effects. Some common side effects include: Eye burning or stinging: A mild burning sensation when the drops are first applied is one of the most common side effects. Redness or irritation in the eyes. Blurry vision immediately after applying the drops. Eye pain or foreign body sensation (a feeling that something is in your eye). Less common side effects may include: Increased eye discharge Infection or injury to the eye (rare) Allergic reactions (rare), including swelling, rash, or itching. Important Considerations: Time to Effectiveness: Restasis typically requires 3 months of regular use to begin showing its full benefits. Pregnancy and Breastfeeding: Talk to your doctor if you are pregnant, plan to become pregnant, or are breastfe3ding, as the safety of Restasis in these situations is not fully established. Contact Lenses: If you wear contact lenses, remove them before using Restasis. Wait at least 15 minutes after using the eye drops before reinserting your lenses. Effectiveness: Restasis helps increase tear production over time, reducing the inflammation associated with dry eye disease. However, it is important to note that Restasis is not a quick-acting solution. It may take a few weeks before you notice improvements, and it should be used regularly as part of your daily routine. The medication can be used long-term to manage chronic dry eye symptoms. Summary: Restasis is a prescription medication that helps treat dry eye disease by reducing inflammation in the eyes and improving tear production. It works over time, often requiring several weeks of use for noticeable benefits. Although it can cause some mild irritation when first applied, Restasis addresses the root cause of dry eyes rather than just providing temporary relief. Always follow Dr. McConkey’s instructions on how to use the medication and when to follow up.
-
CyclosporineThis is generic Restasis. See Restasis for more information.
-
Klarity CKlarity C is a compounded cyclosporine product to treat dry eye, available for patients at a capped price. This is beneficial for patients without prescription insurance coverage to minimize costs.
-
CequaCequa is a cyclosporine product indicated to treat dry eye and increase tear production. More information coming soon. Capped price available at PhilRx Pharmacy
-
VevyeMore information coming soon
-
MieboMore information coming soon
-
XiidraXiidra (generic name: lifitegrast) is a prescription eye drop medication used to treat dry eye disease (DED), a condition in which the eyes do not produce enough tears or the tears evaporate too quickly, leading to inflammation and discomfort. Dry eye disease can cause symptoms such as irritation, a gritty or burning sensation, redness, and excessive tearing as the eye tries to compensate for the dryness. How Xiidra Works: Xiidra works by inhibiting the action of a protein called LFA-1 (lymphocyte function-associated antigen 1), which plays a key role in the inflammation associated with dry eye disease. By blocking LFA-1, Xiidra helps reduce the inflammation in the eye's surface and tear-producing glands, leading to less discomfort and improved tear production. How to Use Xiidra: Dosage: Typically, Xiidra is used twice a day, with one drop in each eye in the morning and evening. Application: Wash your hands before applying the drops. Tilt your head back and pull down your lower eyelid to create a small pocket. Gently squeeze one drop of Xiidra into the pocket of the lower eyelid, being careful not to touch the tip of the dropper to the eye or any surfaces to avoid contamination. Close your eye and gently press your finger to the corner of your eye (near the nose) for about 1-2 minutes to prevent the medication from draining away into the tear duct. If you're using other eye drops, wait about 5 minutes between applying different medications. Possible Side Effects: Like any medication, Xiidra can cause side effects. Some of the most common side effects include: Eye irritation (such as burning or stinging after application) Taste disturbances (a strange or bitter taste in the mouth) Redness or discomfort in the eyes Blurred vision for a short time after applying Less common, but more serious side effects, may include: Eye infection or injury Severe allergic reactions (swelling, rash, etc.) If you experience severe irritation or signs of an allergic reaction, such as swelling of the face or lips, contact your healthcare provider immediately. Considerations and Precautions: Pregnancy and breastfeeding: It's important to discuss the potential risks and benefits of Xiidra with your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. Other medications: Inform your healthcare provider of any other eye medications or systemic medications you are using to avoid interactions. Contact lens users: If you wear contact lenses, remove them before applying Xiidra. Wait at least 15 minutes after using the eye drops before reinserting your lenses. Effectiveness: It may take several weeks of consistent use (typically around 2 weeks or more) before you start to notice significant improvement in your symptoms. For best results, use the drops regularly as prescribed. Xiidra is a valuable treatment option for individuals suffering from moderate to severe dry eye disease, and its anti-inflammatory action helps address the root cause of the condition, offering relief from uncomfortable symptoms. Always follow your doctor’s advice on how to use the medication and when to follow up.
-
TyrvayaTyrvaya (generic name: varenicline solution) is a prescription nasal spray used to treat dry eye disease (DED), specifically for individuals with moderate to severe dry eye symptoms. It is a relatively new treatment that targets the underlying causes of dry eye by stimulating the production of tears through the activation of specific receptors in the nasal cavity, which then help to increase tear production in the eyes. Tyrvaya works by targeting the nicotinic acetylcholine receptors (nAChRs) in the nasal mucosa, which is a unique approach compared to traditional dry eye treatments that focus on lubricating the eyes or reducing inflammation. Key Features of Tyrvaya: Active Ingredient – Varenicline: The active ingredient in Tyrvaya is varenicline, which is a nicotinic acetylcholine receptor agonist. Varenicline is a compound that is best known for its use in smoking cessation medications (like Chantix), but in the case of Tyrvaya, it stimulates tear production by activating receptors in the nasal passages that, in turn, signal the lacrimal glands to produce more tears. Nasal Spray Formulation: Tyrvaya is delivered as a nasal spray, meaning it is administered through the nose rather than the eyes. This delivery method is a novel approach to treating dry eye disease, targeting the body's natural tear production mechanism via the nasal mucosa. Indication: Tyrvaya is used for the treatment of dry eye disease in adults. It is specifically intended for individuals suffering from moderate to severe dry eye symptoms, and it works by increasing natural tear production to alleviate the symptoms of dryness, irritation, and discomfort. How Tyrvaya Works: Tyrvaya stimulates the nicotinic acetylcholine receptors located in the nasal mucosa (inside the nose). When these receptors are activated, they send signals that increase tear production from the lacrimal glands. The increased tear production helps to replenish the tear film, improving moisture and reducing the symptoms of dry eye disease. This mechanism is different from other dry eye treatments, which often focus on lubricating the eye surface or reducing inflammation. How to Use Tyrvaya: Dosage: Tyrvaya is typically prescribed as one spray per nostril twice a day. Application Instructions: Prime the Spray: Before using Tyrvaya for the first time, you need to prime the nasal spray by releasing a few sprays into the air, away from your face, to ensure it delivers a proper dose. Administer the Spray: Tilt the tip toward the ear nearest that nostril Elevate your tongue to the roof of your mouth Administer by pressing the applicator down completely Resist inhaling the mist Visit the following link for video instructions on using Tyrvaya: tyrvaya_en_ifu_1.15 - uploaded 7/11/2024 on Vimeo Consistency: It is important to use Tyrvaya consistently every day, as prescribed by your doctor, for the best results. It may take several weeks for the medication to show noticeable improvements in tear production and dry eye symptoms. Benefits of Tyrvaya: Stimulates Natural Tear Production: Tyrvaya helps stimulate your body’s own tear production, making it a more natural option for treating dry eye symptoms compared to lubricating eye drops, which provide temporary relief. Non-Eye-Based Delivery: Unlike traditional eye drops, Tyrvaya is a nasal spray, which can be a more convenient option for people who experience irritation or discomfort from using eye drops. Long-Term Tear Production: By activating the lacrimal glands to produce more tears, Tyrvaya addresses the root cause of dry eye disease—insufficient tear production—rather than just masking the symptoms. Convenience: Tyrvaya offers a one-daily treatment regimen, making it easier to integrate into your routine. The nasal spray delivery can be more comfortable for some people compared to applying eye drops multiple times a day. Possible Side Effects: While Tyrvaya is generally well-tolerated, there are some potential side effects that may occur, including: Eye Irritation: 8% Temporary blurred vision: 3% Nasal Irritation: Some users may experience irritation or discomfort in the nasal passages, such as a burning or stinging sensation after use. Sneezing: Nasal sprays can sometimes cause sneezing shortly after administration. Headache: Some individuals may experience mild headaches. If you experience persistent or severe side effects, such as severe nasal discomfort, nosebleeds, or signs of an allergic reaction, you should contact your healthcare provider. Considerations and Precautions: Pregnancy and Breastfeeding: The safety of Tyrvaya during pregnancy and breastfeeding has not been fully established. Consult your healthcare provider if you are pregnant, planning to become pregnant, or breastfeeding. Other Medications: Inform your doctor about any other medications or treatments you are using, including over-the-counter or prescription eye drops or nasal sprays, to avoid potential interactions. Allergies: If you have any history of allergic reactions to medications or nasal products, make sure to inform your healthcare provider before using Tyrvaya. Nasal Issues: If you have any history of nasal or sinus conditions (e.g., nasal obstruction, infections), discuss with your doctor whether Tyrvaya is a suitable treatment for you. Conclusion: Tyrvaya is a nasal spray used to treat moderate to severe dry eye disease by stimulating the body’s natural tear production through the activation of nicotinic receptors in the nasal mucosa. By increasing tear production, it provides a more natural and potentially longer-lasting solution to dry eye symptoms compared to traditional eye drops. Tyrvaya offers a convenient once-daily treatment and is an innovative option for those suffering from chronic dry eye. Always follow your healthcare provider’s instructions to ensure the best results and minimize potential side effects.
-
EysuvisEysuvis (loteprednol etabonate ophthalmic suspension) is an effective, short-term treatment for reducing inflammation and pain associated with dry eye disease. By reducing inflammation in the eyes, it helps alleviate discomfort, redness, and irritation, providing significant relief to individuals suffering from acute dry eye symptoms. Its formulation as a soft corticosteroid reduces the risk of common steroid-related side effects, making it a safer choice for short-term use. Always follow your doctor's instructions regarding dosage and duration of use to achieve the best results and minimize the risk of side effects.
-
xDemvyMore information coming soon
-
Autologous Serum TearsAutologous serum tears are a type of eye drop made from your own blood serum and are used as a treatment for severe dry eye disease. They are especially beneficial for individuals with moderate to severe dry eye, particularly when other treatments have not been effective. How They Are Made: Blood Collection: A small amount of your blood is drawn, usually from your arm. Processing: The blood is then processed in a laboratory to separate the serum (the liquid part of the blood) from the red and white blood cells. Preparation: The serum is diluted to a specific concentration (typically around 20%-100% serum) and packaged into sterile vials for use as eye drops. Storage: The drops are typically stored in the fridge and must be used according to the instructions provided by your doctor. Why They Are Used for Dry Eye: Autologous serum tears are used primarily for moderate to severe dry eye cases, often in patients who have not found relief from more conventional treatments like artificial tears, anti-inflammatory eye drops, or other dry eye medications. Benefits: Natural Healing Properties: Serum contains growth factors, nutrients, and proteins (such as vitamin A, epidermal growth factor, and fibronectin) that help promote healing and repair of the eye’s surface. Anti-inflammatory Effects: The serum can have a natural anti-inflammatory effect, which is important in treating inflammation of the eye surface that is often seen in dry eye disease. Mimics Natural Tears: Since they are made from your own blood, autologous serum tears are more closely aligned with the composition of your natural tears and can be highly effective in restoring moisture to the eyes. Beneficial for Severe Cases: They are particularly helpful for people with severe dry eye associated with conditions like Sjögren’s syndrome, graft-versus-host disease (GVHD), severe Meibomian gland dysfunction, or chemical burns. How Autologous Serum Tears Help: Moisturizing: They provide long-lasting moisture for the eyes, helping to alleviate the discomfort of dryness. Promoting Corneal Healing: For individuals with damage to the corneal surface, the growth factors in serum tears support tissue repair and healing. Reducing Inflammation: Serum has natural anti-inflammatory properties that can reduce the inflammation that often accompanies dry eye disease. Who Can Benefit from Autologous Serum Tears? Autologous serum tears are typically considered when other treatments (like artificial tears or anti-inflammatory medications) are not effective. Common candidates for serum tears include: People with severe dry eye conditions (often with underlying health issues like Sjögren’s syndrome). People who have corneal damage or epithelial defects (due to conditions like ocular surface disease, chemical burns, or post-surgical recovery). People who are undergoing treatments that exacerbate dry eye, such as chemotherapy or graft-versus-host disease (GVHD). Possible Side Effects: Irritation or discomfort: Some people may experience mild irritation or burning when using serum drops. Risk of infection: As with any eye treatment, there is a risk of contamination, so it’s important to follow hygiene guidelines when handling the serum vials. Storage requirements: Autologous serum must be stored in a refrigerator, and improper storage can lead to degradation of the serum, making it ineffective. Conclusion: Autologous serum tears are a specialized treatment for individuals with severe dry eye disease, especially when conventional treatments are insufficient. Because they are derived from the patient’s own blood, they contain natural healing factors that can help promote eye surface repair, reduce inflammation, and provide long-lasting moisture. However, they should be used under the guidance of an eye care professional due to their specific preparation and storage requirements.
-
OxervateOxervate (generic name: cenegermin) is a prescription eye drop used for the treatment of neurotrophic keratitis (NK), a rare and serious condition that affects the cornea of the eye. Neurotrophic keratitis occurs when there is damage to the corneal nerves, leading to a reduction in corneal sensitivity, poor healing, and impaired tear production. This can result in symptoms like corneal ulcers, pain, blurred vision, and increased risk of infection. How Oxervate Works: Oxervate contains cenegermin, which is a recombinant form of nerve growth factor (NGF). NGF plays a crucial role in the survival, growth, and maintenance of nerve cells, particularly the corneal nerves. By promoting nerve regeneration and repair, Oxervate helps to restore corneal sensitivity and supports the healing process of the corneal surface. Nerve Regeneration: The active ingredient in Oxervate, nerve growth factor, helps stimulate the regeneration of corneal nerves that may have been damaged or are not functioning properly due to neurotrophic keratitis. Improved Healing: NGF promotes healing of the corneal epithelium (the outermost layer of the cornea), allowing the cornea to recover from any damage or ulcers that may have occurred due to the lack of nerve function. Restoring Sensitivity: By improving corneal nerve function, Oxervate helps restore normal corneal sensitivity, reducing the risk of further injury and promoting the normal production of tears. Indication: Oxervate is specifically indicated for the treatment of neurotrophic keratitis (NK) in adults. NK is typically associated with conditions that damage the trigeminal nerve or impair corneal nerve function, such as: Herpes simplex virus (HSV) infection. Diabetes (which can lead to nerve damage). Chemical burns. Refractive surgery (like LASIK) that can affect the corneal nerves. How to Use Oxervate: Dosage: Oxervate is typically prescribed as one drop in the affected eye six times per day (about every 2 hours during waking hours) for a period of 8 weeks. Application: The drops should be instilled directly into the affected eye(s), and patients are advised to avoid touching the tip of the dropper to the eye or surrounding areas to prevent contamination. Storage: Oxervate should be stored in the refrigerator and used within 28 days after opening the bottle. If the bottle is not used within this time frame, it should be discarded. Potential Side Effects: Common side effects of Oxervate are generally mild and may include: Eye irritation or discomfort. Conjunctival hyperemia (redness of the eye). Eye pain. Foreign body sensation (feeling like something is in the eye). Eyelid swelling or itching. In rare cases, more serious side effects could occur, but these are typically uncommon. It’s important to follow the prescribed dosage and instructions to minimize the risk of side effects. Effectiveness: Oxervate has been shown to be effective in promoting corneal healing and improving corneal sensitivity in patients with neurotrophic keratitis. Clinical trials have demonstrated that patients treated with Oxervate have a higher rate of healing of corneal ulcers and a reduced risk of complications compared to those who do not receive NGF therapy. Many patients experience significant improvement in symptoms and corneal integrity after the treatment period. Conclusion: Oxervate (cenegermin) is an important treatment option for neurotrophic keratitis, as it helps to stimulate corneal nerve regeneration and improve the healing of corneal ulcers. It provides a novel approach to treating a condition that previously had limited treatment options, especially for patients suffering from nerve-related corneal damage. As with any medication, it’s important to use Oxervate under the guidance of an eye care professional to ensure it’s used correctly and effectively.
-
Lubricating Drops and OintmentsArtificial Tears lubricate the eye. They are an important aspect of dry eye therapy and may alleviate symptoms temporarily, however, they do not treat the underlying cause. There are many types of over-the-counter Dry Eye drops. We recommend only using preservative free artificial tears, as many dry eye patients are sensitive to common preservatives. Tears: Basic lubricating drops Oil Based Tears: Helpful in patients with evaporative dry eye Gel Drops: Stay on the eye longer for an extended effect, but may blur vision Ointments: Best for nighttime use, will blur the vision but help in patients with incomplete eyelid closure and lubricate while you are sleeping
-
Hot CompressesThe tear film has three layers, mucous, water, and oil. The top oil layer prevents the tears from evaporating and is secreted by glands in the eyelid, called Meibomian glands. Applying a moist heat compress to the eyelids for 8-10 minutes, twice daily, is proven to melt the secretions of the meibomian glands and improve tear quality. Meibomian glands can get clogged due to a number of reasons, and it is always best to see an eye doctor to rule out the underlying cause. If the glands get clogged and infected, a stye can occur, and applying moist heat is vital to unclog the oil gland. Dr. McConkey recommends the Optase Moist Heat mask. If microwaving a mask is not an option or is inconvenient, there are rechargeable or single use masks available.
-
Lid ScrubsThe eyelids and lashes can house microorganisms including demodex mites and bacteria, which can clog the meibomian glands and cause inflammation of the eyelid and ocular surface. Cleaning the eyelids is an important aspect of dry eye treatment. There are a variety of lid foams, gels, and wipes available over the counter. We do not recommend using baby shampoo, as this is an outdated recommendation.
-
Sleep MaskSleep masks are a great way to protect the eyes while you are sleeping from fans and incomplete eyelid closure.
-
Sleep MasksMany people do not close their eyes completely when they sleep at night, causing dryness that is worse in the morning. These symptoms are worsened if you sleep with a fan. One way to combat this type of dry eye is to wear a sleep mask at bedtime. If you cannot tolerate a sleep mask, another option is ointment.
-
Do You See Children?We do not have an age limit on the patients we see, however, we will only see children who have a need for our practice. We focus on Dry Eye and Medically Necessary Contact Lenses, so we will see pediatric patients who have a stye or keratoconus, but do not perform routine eye exams. We will also see children with urgent care needs such as a scratched or red eye. For pediatric eye doctors in Harford or Baltimore Counties, please check out this quick guide we made for your convenience.
-
Do you accept Vision Plans?We accept VSP, Spectera, and some Eyemed plans for medically necessary contact lenses only. In order to qualify for Medically Necessary Contact Lenses, you must meet the requirements of your individual vision plan, which varies by company. We do not perform routine vision exams. All exams outside of Medically Necessary Contact Lens Fittings are billed through medical insurance and susceptible to your deductible, copays, and coinsurance.
-
What medical insurances do you accept?Medicare Blue Cross Blue Shield BlueChoice Carefirst Administrators Alterwood Health Cigna Aetna United Healthcare (except EPO) MultiPlan We do not accept any medical assistance plans as of 1/1/2025
-
Where do I purchase more dry eye products?McConkey Eye Care offers products in office and online. We have competitive pricing to allow you to support our small business in a way that is convenient for you. Given the frequent recalls of dry eye products, we aim to ensure our patients are purchasing their dry eye products from a reputable source.
-
Do you perform routine eye exams?No, we do not perform routine eye exams. We see patients for Dry Eye and Medically Necessary contact lenses, such as RGPs and Scleral lenses.
-
Does your office have an optical?No, our office does not have an optical. We would be happy to refer you to a colleague for a great pair of glasses! Just ask one of our staff members today!










_edited.jpg)




